MRI NEWSLETTER: Patella Dislocation
Posted May 8, 2018
Patella disclocations are very common especially in soccer players. The history is frequently ‘rule out ACL tear’. The highest pre-test probability is females 10 to 40 years of age.
The most common mechanism is sudden twisting. The classic MRI findings of lateral patella dislocation syndrome is contusion of the inferior-medial patella facet and contusion of the anterior-lateral femoral condyle. Commonly there is tearing of the medial patella femoral ligament. In 10% of cases there is an osteochondral fracture.
The primary medial stabiliser of the patella is the medial patella-femoral ligament, MPFL. More inferiorly is the medial patella-tibial ligament, MPTL, which is a secondary stabilizer of the patella.
MPFL extends from the superior patella to the medial collateral ligament located between adductor tubercle and the medial epicondyle. 10% of MPFL tears are proximal, 60% are multifocal and 17% are distal.
Young soccer player
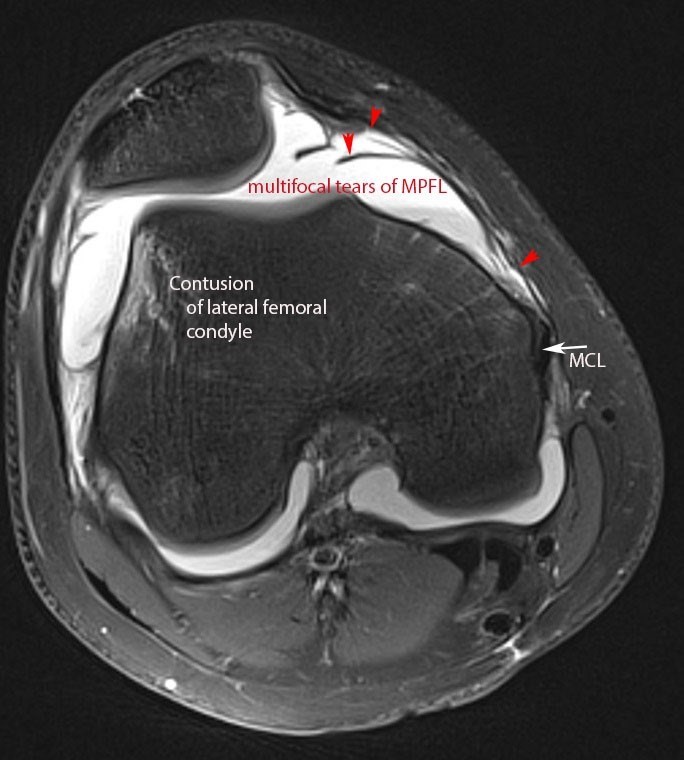
Patellar dislocation syndrome
Axial view: Contusion of the anterior-lateral femoral condyle, lateral displacement of patella, multifocal tears of MPFL, MCL. Fluif-fluid level is due to blood in joint.
Coronal PD fat-sat: contusion of the anterior-lateral femoral condyle, osteochondral fragment and donor site of osteochondral fracture fragment, large joint effusion
The most recent recommendation for surgery is to obtain an MRI after transient patella dislocation. If no osteochondral defect is present, the patient should be treated with physical therapy. The physical therapy should strengthen the vastus medialis and gluteal muscles.
If there is a second dislocation, the patient should be treated with surgery. The most recent trend in reconstruction of the knee is to repair both the primary stabiliser, the MPFL, and the second secondary medial stabiliser, the MPTL. This is performed by taking a thin section of the patella tendon inferiorly. These sections are attached to the medial portion of the knee.
Read the full article here: Patella Dislocation
By Dr William Renner
